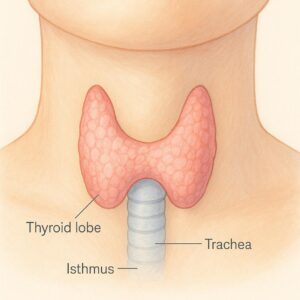
Hashimoto’s Thyroiditis is an autoimmune disorder in which the immune system mistakenly attacks the thyroid gland. This leads to chronic inflammation and often results in hypothyroidism, where the thyroid produces too little hormone. Common symptoms include fatigue, weight gain, cold intolerance, dry skin, depression, and brain fog. It’s more common in women and typically develops gradually over time. Hashimoto’s is diagnosed through blood tests (checking TSH, free T4, and thyroid antibodies) and is usually treated with thyroid hormone replacement therapy (like levothyroxine).