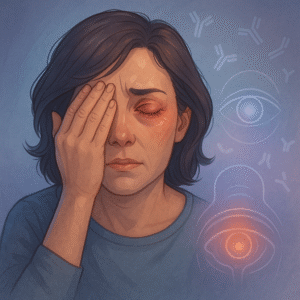
Autoimmune uveitis is a type of eye inflammation caused by the immune system attacking parts of the eye—especially the uvea, which includes the iris, ciliary body, and choroid. This condition can cause eye pain, redness, blurry vision, and even vision loss if not treated. It may occur on its own or as part of a systemic autoimmune disease.