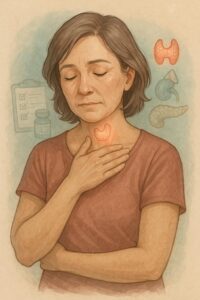
Autoimmune Polyendocrine Syndrome Type 2 (APS-2) is a chronic autoimmune disorder in which the immune system attacks multiple endocrine glands, especially the adrenal glands, thyroid gland, and pancreas. It most often includes:
-
Addison’s disease (adrenal insufficiency)
-
Autoimmune thyroid disease (like Hashimoto’s or Graves’)
-
Type 1 diabetes
Unlike APS-1 (which is rare and genetic), APS-2 is more common, usually develops in adulthood, and is not linked to a single gene mutation.